
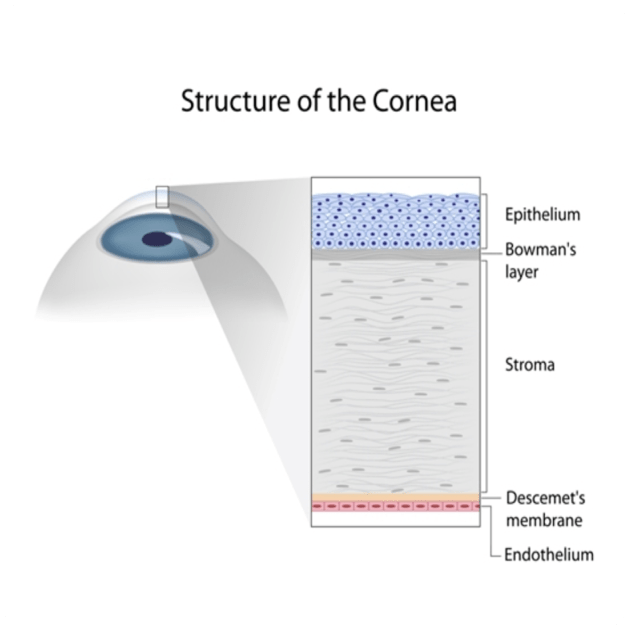
The human eye is a marvel of nature, a complex organ that allows us to perceive the world around us. However, several conditions can compromise our vision, one of them being corneal disease. The cornea is the clear dome-shaped front surface of the eye and is comprised of 5 layers, from the outermost epithelium layer to the innermost endothelium layer.
If the cornea is damaged or diseased, it can severely impair vision. The journey to clearer vision often leads patients with corneal diseases down the path of needing a corneal transplant.
Corneal transplantation, also known as keratoplasty or corneal graft, is a surgical procedure in which a damaged or diseased cornea is replaced with a healthy donor cornea. When most people think of corneal graft surgery, they think of the traditional procedure where the entire central cornea is removed and replaced with a donor cornea. However, the field of corneal transplantation has evolved significantly over the years so this type of full-thickness corneal transplantation is performed less frequently. We now have more refined techniques that have allowed us to replace only the diseased layers of the cornea in the majority of cases depending on a patient’s eye condition.
There are three main types of corneal transplants, Penetrating Keratoplasty (PK), Endothelial Keratoplasty (EK) and Deep Anterior Lamellar Keratoplasty (DALK) each with their own indications, benefits and limitations.
Corneal Transplant technique | Description | Benefits | Limitations |
Penetrating Keratoplasty (PK) | PK is the traditional method of corneal transplantation where the entire central cornea is replaced with a donor cornea. The surgeon uses sutures to secure the graft in place. This procedure is typically used for conditions that affect all layers of the cornea such as severe keratoconus, scars or infection | Proven effective for a wide range of corneal diseases | Invasive procedure Higher risk of graft rejection Sutures often lead to postoperative astigmatism and increase the risk for corneal infection |
Endothelial Keratoplasty (EK) | EK procedures replace only the damaged innermost layer of the cornea, known as the endothelium, leaving he front layers intact. There are two types of EK, Descemet’s Membrane EK (DMEK) and Descemet’s Stripping EK (DSEK or DSAEK). These procedures are primarily used to treat conditions where the endothelial cells are dysfunctional, such as Fuch’s Endothelial Dystrophy and Bullous Keratopathy. | Minimally invasive procedure compared to PK and DALK. Faster visual recovery. Lower risk of graft rejection. Less risk of postoperative astigmatism.
| More challenging and specialised surgical skills required. Limited to a small range of corneal conditions only effecting the endothelial layer.
|
Deep Anterior Lamellar Keratoplasty (DALK) | DALK, often referred to as a partial thickness corneal transplant, involves the replacement of the anterior surface of the cornea, whilst leaving the healthy endothelium layer intact. DALK is typically chosen when the innermost layers of the cornea are healthy, but the outermost layers are affected, as seen in conditions like mild keratoconus and corneal scarring | Preserves the natural endothelium layer reducing the risk of graft rejection Lower risk of intraocular infection compared to PK. May be repeated without increasing the risk for rejection | Technically demanding procedure. Sutures may lead to postoperative astigmatism and increase the risk for corneal astigmatism |
PK, EK and DALK all have the same goal of restoring vision, but they differ in their indication, technique, recovery and potential outcomes. While PK has traditionally been the gold standard for corneal transplantation, EK and DALK procedures are increasingly favoured due to their faster recovery times and lower complication rates. Ultimately, the decision should be based on a thorough evaluation by an experienced Ophthalmologist, who can recommend the most suitable corneal transplant option for your eye condition.
Copyright © 2023 Nexus Eye Care | Trans4m Business Consulting – Website Design & SEO | Privacy Policy | ^