Diabetes is a well-known condition that affects how your body processes glucose. Elevated blood sugar levels can lead to serious health complications if not managed properly, and this includes diabetic eye disease. In this blog, retinal specialist Dr Anagha Vaze discusses the impact diabetes can have on the eye and what you can do to protect your eyesight.
Diabetes can affect the body in many ways, but the eyes are particularly vulnerable. As a retinal specialist, I regularly encounter a variety of eye conditions caused by diabetes.
Diabetic eye disease is a group of eye conditions that people with diabetes are at an increased risk of developing and, if left untreated, can lead to vision loss or blindness. Fortunately, the majority of diabetes-related vision loss can be avoided if detected early.
In the short term, you are not likely to have permanent vision loss due to high sugar levels. Vision may be intermittently blurry due to fluctuating sugar levels, but usually settles as they become more stable. People with diabetes also have an increased risk of some types of glaucoma and early cataract development. The longer the duration of diabetes or poor control of blood sugar levels, the greater the risk of damage to blood vessels throughout the body, including those in the eye; this is known as diabetic retinopathy.
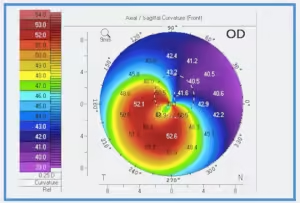
Diabetic retinopathy is the most common form of diabetic eye disease. It affects the blood vessels in the retina, the light-sensitive tissue that lines the back of the eye. The primary cause of diabetic retinopathy is exposure of the retina to high levels of glucose in the blood, and the severity of the disease is greatly influenced by how well your diabetes is controlled. Unfortunately, it is possible to develop diabetic retinopathy even when your blood sugar levels are well controlled. This is why regular diabetic eye examinations are so important to detect diabetic retinopathy early.
Diabetic retinopathy can affect the retina in the following ways:

NPDR is divided into 3 stages; mild, moderate, and severe. Mild NPDR often presents with no noticeable symptoms. At this point, the blood vessels in the retina start to weaken and develop tiny bulges called microaneurysms. As the disease progresses, the blood vessels become blocked, which can lead to swelling in the retina. In the later stages of NPDR, blood vessels supplying the retina can become blocked, resulting in reduced blood supply to the eye. The body then attempts to compensate by growing new, abnormal blood vessels in the retina; however, these new vessels are fragile and can break easily, causing bleeding.
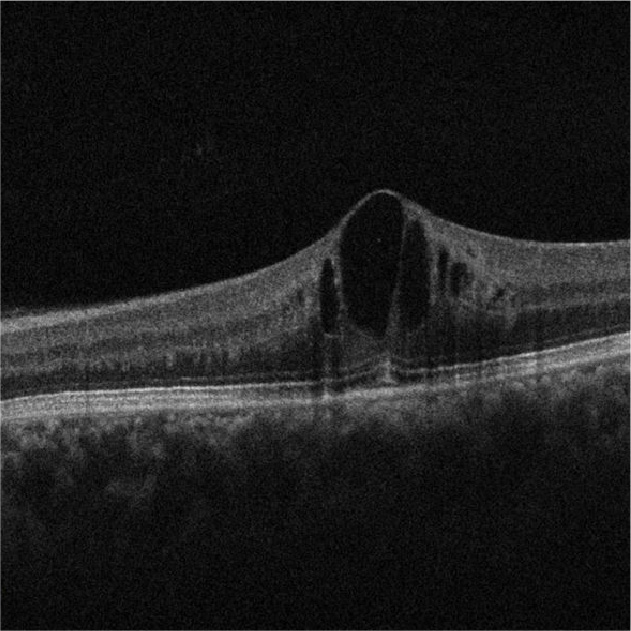
DME is caused by fluid accumulation in the macula, leading to swelling and thickening. It can cause blurry, patchy, and/or distorted vision. DME can occur at any stage of diabetic retinopathy and is a leading cause of central vision loss in diabetic patients. If diagnosed early, diabetic macular edema often responds well to treatment, and vision can potentially be regained.
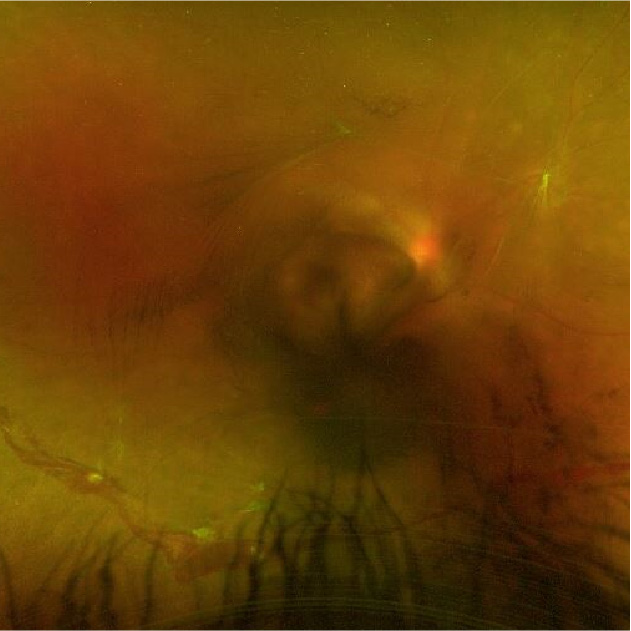
PDR is the most advanced stage of diabetic retinopathy. In this stage, there is more widespread damage to retinal blood vessels; abnormal blood vessels continue to grow and can extend into the vitreous gel inside the eye, causing vitreous haemorrhage and severely reduced vision. Scarring can occur, and as the scar contracts, this can lead to retinal detachment and permanent vision loss, requiring urgent surgical treatment by a retinal specialist.
Treatment of diabetic retinopathy depends on the stage and severity of the disease. Fortunately, several effective treatment options are available to manage and, in some cases, reverse diabetic retinopathy. In most cases, the earlier diabetic retinopathy is diagnosed, the more successful the treatment can be. Later stages have a poorer visual prognosis and may require surgical management by a retinal specialist.
In its early stages, when vision is usually unaffected, improved blood sugar levels and blood pressure control, as well as lifestyle changes such as diet and exercise, can be very effective in preventing disease progression. You will need to see an eye specialist for close monitoring every three to twelve months, depending on the severity of the disease.
For later stages, treatment by a retinal specialist includes:
People with diabetes can significantly reduce their risk of diabetic eye disease by carefully managing their blood sugar levels. This includes regular monitoring, a balanced diet, exercise, and taking medication as prescribed by a health care professional. Optimising all other cardiovascular risk factors, mainly blood pressure and cholesterol, is also important. Maintaining regular eye examinations, even if you don’t have any symptoms, can significantly reduce the risk and severity of eye complications.
Prevention, early detection, and timely treatment are crucial to managing diabetic eye disease and preventing vision loss. As a retinal specialist, I urge everyone living with diabetes to prioritize regular eye examinations and work closely with their healthcare team to maintain good blood sugar control.
Dr Anagha Vaze is an Ophthalmologist and retinal specialist with subspecialty training in medical retina, uveitis, and inherited eye disorders. Dr Vaze is a highly experienced surgeon, consulting at Nexus Eyecare Norwest and Nexuse Eyecare Blacktown.
Copyright © 2023 Nexus Eye Care | Trans4m Business Consulting – Website Design & SEO | Privacy Policy | ^